-
Centre of
Excellence
Centre of Excellence
- Accident and Emergency Care
- Cancer Care/Oncology
- Cardiology
- Cardiothoracic Vascular Surgery
- Gastrointestinal Science
- Laparoscopic Surgery
- Liver Transplantation Surgery
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Organ Transplant
- Orthopaedics
- Paediatric And Child Care
- Rheumatology
- Spine Care
- Urology
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Bone Marrow Transplantation
- Children’s Airway & Swallowing Centre
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Genetics
- Geriatric Medicine
- GI Surgery
- Gynaec Oncology
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Laboratory Medicine
- Lactation
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Cancer Care
- Paediatric Cardiology
- Paediatric Endocrinology
- Paediatric General Surgery
- Paediatric Intensive Care Unit
- Paediatric Neurology
- Paediatric Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pediatric Bone Marrow Transplant
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Psychology
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Rehabilitation Medicine
- Renal Sciences
- Reproductive Medicine
- Robotic Assisted Surgery
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
- Doctors
- Mukundapur
-

Bengaluru

-
-

Bhubaneswar

-

Bhubaneswar
-
-

Delhi - NCR

-

Goa

-

Goa
-
-

Jaipur
-

Kolkata

-

Mangaluru
-

Mysuru
-

Patiala
-

Pune

-

Ranchi
-

Salem
-

Siliguri City

-

Vijayawada
- International Patients



Clinics







- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Whipple
Whipple Procedure in Mukundapur
A Pancreaticoduodenectomy, also referred to as Whipple Surgery, is an advanced surgical procedure primarily used for the treatment of pancreatic cancer located in the pancreatic head. During the procedure, a large portion of the duodenum (the first part of the small intestine) and adjacent lymph nodes, as well as the gallbladder and pancreas head, are removed.
In more complicated cases, the treatment may include the removal of additional tissues along with portions of the stomach and pancreatic body. Due to its intricacy, the course of therapy typically lasts six hours, though this can change based on the individual patient and the difficulty of the surgery. Following surgery, patients typically need to stay in the hospital for one to two weeks.
At Manipal Hospitals, Mukundapur, the Surgical Gastro Department is equipped to carry out Whipple Procedure for patients with pancreatic or other gastrointestinal cancers, ensuring personalised treatment plans, meticulous surgical precision, and comprehensive postoperative care.
FAQ's
-
Pancreatic cancer is a type of cancer that affects the pancreas and interferes with its function to help digest food and produce hormones. As a result, patients develop symptoms such as jaundice, stomach pain, and weight loss.
-
Risk factors include smoking, obesity, and family history. Surgery, Chemotherapy, or Radiation Therapy are the existing treatment modalities and are performed depending on the cancer stage. Despite improvements, the prognosis of pancreatic cancer remains challenging, and improved outcomes are contingent upon early identification.
The pancreas, a fish-shaped gland, is a vital organ in the abdomen. Its head is the biggest part on the right, and it tapers down to a thin tail before transitioning into the neck or body in the middle. The pancreas is a multipurpose organ that aids in the production of hormones, helps in digestion, and regulates blood sugar.
The exocrine function of the gland includes producing digestive enzymes that help the small intestine break down fats, proteins, and carbohydrates; the endocrine function of the gland involves secreting glucagon and insulin to control glucose metabolism. This dual function highlights how crucial the pancreas is to maintaining overall health and metabolic equilibrium.
In addition to pancreatic cancer, other conditions include ampullary cancer, bile duct cancer, pancreatic cysts, pancreatitis, duodenal small bowel cancer, pancreatic or small intestinal injury, and neuroendocrine tumours that may also necessitate the Whipple Procedure. This complex procedure targets abnormalities affecting the pancreas, bile duct, duodenum, and adjacent tissues to reduce symptoms and improve patient outcomes. The procedure's versatility not only treats pancreatic cancer but also a range of challenging conditions affecting the abdominal region through surgery.
Before undergoing the Whipple procedure, cancer patients often get Chemotherapy or Radiation Therapy to regulate their condition. Pre-surgery protocols typically entail tapering off on certain medications and abstaining from food and liquids for eight hours before hospital admission. It is advised to give up smoking, even for a brief period, to enhance heart and lung health. Herbal supplements and erectile dysfunction medications should be stopped as directed at least 24 hours before surgery. Certain blood pressure medications can be continued as per a doctor's order. When you first arrive at the hospital, an intravenous line (IV) is placed so that you can receive fluids and medication.
Open surgery makes use of a single, bigger incision, while laparoscopic or minimally invasive surgery makes use of several smaller ones. However, because the Whipple procedure is so intricate and requires precise manipulation of numerous organs and tissues, it frequently requires an open approach. Although less intrusive techniques offer advantages such as reduced bleeding and faster healing, the intricacies of Whipple surgery often necessitate the enhanced vision and agility that come with an open surgical approach. As a result, patients receive the best possible care because surgeons can more adeptly manage and navigate the challenges associated with pancreatic and adjacent organ involvement.
The infamously challenging Whipple procedure can take four to twelve hours, depending on a variety of factors, such as the overall health of the patient, the extent of the illness, and the surgical intricacies. This surgical treatment involves carefully dissecting and removing diseased pancreatic tissue, surrounding organs, and lymph nodes to preserve critical structures. The requirement for surgeons to precisely navigate intricate anatomical components in order to get the optimum results explains the differences in surgical duration seen in Whipple surgeries. This is a lengthy procedure that is necessary to improve the prognosis and quality of life for patients with certain pancreatic and periampullary tumours.
Following the Whipple procedure, up to one-third of patients encounter a range of problems, including fistula issues, bowel leaks, organ leaks, bleeding, infection, and either temporary or chronic diabetes. Additionally, patients may experience difficulties with some meals' digestion, which can result in bowel irregularities and weight loss. Constipation is one of the other potential side effects, which makes sense considering the significant physiological impact this complex surgical treatment has on gastrointestinal function and metabolic balance. Close observation and postoperative care are essential to address and minimise these problems, as well as to give patients the best recovery and long-term health outcomes.
After the Whipple procedure, patients usually start with a clear liquid diet in the early postoperative days and gradually transition to solid foods under the physician's supervision. Soft foods that are simple to digest become essential for minimising gastrointestinal discomfort and promoting healing throughout this recovery phase. Patients must discuss recommended food options with their healthcare provider to ensure their dietary choices fit their unique postoperative needs and preferences. Optimising nutritional intake can lower any serious complications and accelerate recovery.
Home Mukundapur Specialities Surgical-gastro Whipple-treatment

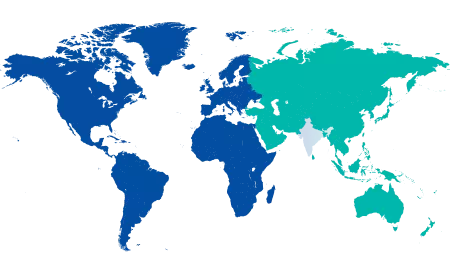
You’re on Our Indian Website
Visit the Global site for International patient services
Your Feedback is Highly Valued!






