-
Centre of
Excellence
Centre of Excellence
- Accident and Emergency Care
- Cancer Care/Oncology
- Cardiology
- Cardiothoracic Vascular Surgery
- Gastrointestinal Science
- Laparoscopic Surgery
- Liver Transplantation Surgery
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Organ Transplant
- Orthopaedics
- Paediatric And Child Care
- Rheumatology
- Spine Care
- Urology
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Bone Marrow Transplantation
- Children’s Airway & Swallowing Centre
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Genetics
- Geriatric Medicine
- GI Surgery
- Gynaec Oncology
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Laboratory Medicine
- Lactation
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Cancer Care
- Paediatric Cardiology
- Paediatric Endocrinology
- Paediatric General Surgery
- Paediatric Intensive Care Unit
- Paediatric Neurology
- Paediatric Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pediatric Bone Marrow Transplant
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Psychology
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Rehabilitation Medicine
- Renal Sciences
- Reproductive Medicine
- Robotic Assisted Surgery
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
- Doctors
- Mukundapur
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Testicular Cancer
Testicular Treatment Hospital in Mukundapur
Uncontrollably growing abnormal cells in the testicles cause testicular cancer. Although it can happen at any age, it is more frequent in young men between the ages of 15 and 35. Although the precise aetiology is uncertain, risk factors include genetic disorders such as Klinefelter syndrome, undescended testicles (cryptorchidism), and family history. A painless lump or swelling in the testicle, pain or discomfort in the scrotum or testicle, a sensation of weight in the scrotum, and backache are possible symptoms.
Alpha-fetoprotein (AFP), beta-human chorionic gonadotropin (β-hCG), and lactate dehydrogenase (LDH) are among the tumour indicators that are measured during physical examinations, blood tests, and ultrasounds used in the diagnosis process. Depending on the kind and stage of the cancer, treatment options may include Radiation Therapy, Chemotherapy, and Surgery to remove the afflicted testicle (radical inguinal orchiectomy). Testicular cancer has a high chance of cure, with over 95% five-year survival rates when detected and treated early.
Specialists at the Urology Department at Manipal Hospitals' Centre for Testicular Treatment in Mukundapur, Kolkata, provide expert guidance for patients with testicular cancer, providing necessary support from diagnosis to follow-up care throughout their treatment journey.
FAQ's
Age (15–35 years old), cryptorchidism, family history, prior testicular cancer, genetic disorders such as Klinefelter syndrome, white race, HIV infection, exposure to the environment, and testicular trauma are common risk factors for testicular cancer. Even though these factors raise the risk, many instances don't have any identified risk factors. Effective treatment and better results depend on early diagnosis.
The majority of males diagnosed with testicular cancer are young and middle-aged, usually between the ages of 15 and 35. However, testicular cancer can be diagnosed in anyone at any age, including elderly men. Especially for males in this age group, regular self-examinations and symptom awareness are essential for early discovery since timely diagnosis and treatment can improve results.
Testicular swelling or painless lumps are common signs of testicular cancer. Other symptoms include scrotal pain or discomfort, a heaviness sensation, changes in testicle size or form, lower abdominal or groyne pressure, and back pain if the disease has progressed. Since not all men have symptoms, it is crucial to regularly examine oneself and seek medical assistance if there are any alarming changes. Effective therapy depends on early discovery.
When diagnosing testicular cancer, a complete physical examination is performed to look for lumps, and then imaging, such as ultrasound, is used to see the masses. Tumour markers (AFP, β-hCG, LDH) are measured by blood tests to help in diagnosis and therapy monitoring. To determine the extent or spread of the cancer, imaging tests such as Computed Tomography (CT) scans, Magnetic Resonance Imaging (MRI), or Positron Emission Tomography (PET) scans may be used. Although rare for testicular cancer due to the risk of spreading, a biopsy might be considered in certain cases.
Testicular cancer includes both germ cell tumours (GCTs) and non-germ cell tumours, which include seminomas and non-seminomas, such as teratoma and embryonal carcinoma. Staging helps in making treatment decisions; adjuvant therapy or monitoring may be utilised for Stage I, while systemic Chemotherapy may be used for Stage III. Treatment methods, including Radiation Therapy, Chemotherapy, and Surgery, are tailored to the patient's unique traits and the characteristics of the cancer to provide the best possible outcome and long-term surveillance for side effects and recurrence.
What surgical options are available for treating testicular cancer, and when is each type indicated?
-
Radical Orchiectomy: This procedure involves the removal of the affected testicle and is the primary treatment for testicular cancer, regardless of the stage. It is typically performed for early-stage cancer to confirm the diagnosis and remove the primary tumour.
-
Retroperitoneal Lymph Node Dissection (RPLND): This surgery is recommended for patients with Stage II testicular cancer when the cancer has spread to the lymph nodes in the retroperitoneum. RPLND involves the removal of lymph nodes to check for cancerous cells. There are two approaches:
-
Standard RPLND: Removes a larger number of lymph nodes.
-
Modified RPLND: A less extensive procedure that selectively removes only those lymph nodes that are most likely to contain cancer.
-
Testicular Sparing Surgery: In cases of localised or extragonadal tumours where preserving the testicle is feasible, surgery may involve removing only the tumour and preserving the surrounding testicular tissue. This approach is rare and generally used in specific situations where the cancer is localised and testicle preservation is deemed possible.
The main treatment for metastatic or advanced testicular cancer is Chemotherapy, which kills cancer cells all across the body. Combinations based on Cisplatin are often used in regimens. When high-energy beams are used to target cancer cells, radiation treatment works well for seminomas. These therapies can be applied as adjuvant therapy or in conjunction with surgery. The kind, stage, and preferences of the patient all influence the decision. Treatment strategies are tailored by multidisciplinary teams to maximise results and minimise negative effects.
Testicular cancer prognosis is much improved by early discovery, which guarantees timely care while the illness is localised and more manageable. Because of its low occurrence, regular screening is not recommended; nonetheless, it is critical to recognise the symptoms. Men should self-examine regularly and notify their healthcare practitioner of any changes. For people who are considered high-risk, such as those with a family history of cryptorchidism, screening may be advised. Self-examination education is still essential for prompt diagnosis and treatment.
Long-term consequences of testicular cancer therapy include infertility, hormone abnormalities, heart problems, secondary malignancies, neurotoxicity, psychological effects, dysphoria, and exhaustion. Hormone replacement treatment, sperm banking, frequent monitoring, lifestyle changes, medication, counselling, and survivorship care are some of the management techniques. To effectively address the unique needs of survivors and maximise their long-term well-being, multidisciplinary approaches involving diverse professionals are essential.
Home Mukundapur Specialities Urology Testicular-cancer

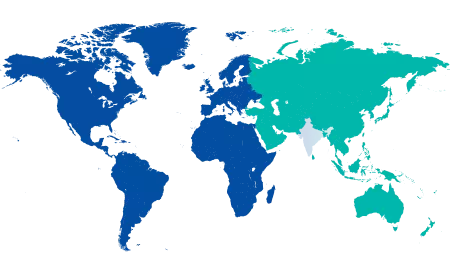
You’re on Our Indian Website
Visit the Global site for International patient services










