Human Papillomavirus (HPV) is one of the most common sexually transmitted infections (STIs), yet it remains surrounded by myths and misconceptions. Questions about symptoms, transmission, and cancer risk are common when trying to understand HPV. Gaining a clearer understanding can help protect your health and your partner's. This blog debunks common HPV myths and provides evidence-based facts to empower you with knowledge.
9 Myths and Facts of HPV:
HPV, or Human Papillomavirus, is a common sexually transmitted infection (STI). Most individuals who are sexually active will contract HPV at some point in their lives. While most low-risk HPV infections resolve on their own, some types can lead to serious health concerns, like cervical, anal, and oral cancers.
Now, the question lies: Can we prevent HPV? The answer would be YES… through HPV vaccination. It is highly effective in preventing infection from high-risk strains of the virus that can potentially cause malignancy. However, not everyone is aware of this protective shield, and even if some are, they’re surrounded by a lot of misinformation about HPV vaccination and, in general, cervical cancer. So, let’s debunk a few common myths about HPV:
Myth 1: HPV Is Uncommon
Fact:
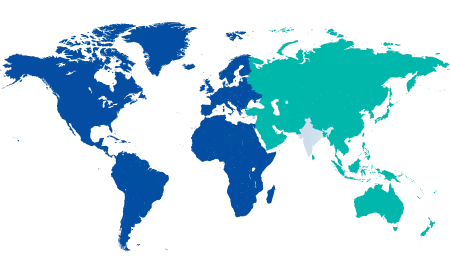
HPV is one of the most common STIs in the world. There’s an 80% chance you’ll get HPV if you’re sexually active. HPV often causes no symptoms, and many people don’t even realize they are infected until it manifests as cancer, for example, cervical cancer. This is one more reason why regular screening is important, besides getting vaccinated.
Explanation:
HPV is not a sign of a lifestyle choice—it’s a prevalent virus. Detection is further complicated by its ability to remain dormant in the body for years, often showing no symptoms. Pap smears and HPV tests can detect infections when they are still mild and when complications are least likely.
Myth 2: No Symptoms Means No HPV
Fact:
Often, there are no symptoms associated with HPV infections; your body can carry the virus without your knowledge. Most strains of HPV cause no symptoms, and only a few, known as high-risk types that are associated with cancers, produce symptoms that can be seen, such as warts, but remain chronically unrecognized before significant cellular changes occur.
Explanation:
Vaccinations and screenings are essential because HPV often progresses without noticeable symptoms. HPV tests can find high-risk strains, while Pap smears can find abnormal cervical cells. Early intervention is possible with these preventive measures before the virus becomes a severe health problem.
Myth 3: HPV can Only Be Spread by Sexual Intercourse
Fact:
Direct skin-to-skin intimate contact is how you contract HPV. Most transmissions happen during sexual activity, but it is possible to transmit through non-sexual skin-to-skin contact, such as touching a wart or an infected area. The virus can also pass from mother to child during childbirth.
Explanation:
This is why you need to understand transmission routes and the need for comprehensive preventive strategies (use of barrier contraceptives). Although they reduce the risk, they don’t cover all genital areas, so there is still a risk of transmission. Your best defense against high-risk HPV strains is vaccination.
Myth 4: HPV isn't a Serious Health Problem
Fact:
Some high-risk HPV strains are associated with several cancers, including cervical, anal and oropharyngeal cancers.
Explanation:
Most HPV infections sort themselves out on their own, but persistent infections with high-risk strains may lead to pre-cancerous lesions and cancer. Regular Pap tests and HPV tests can help catch abnormal cells early and improve your reproductive health.
Myth 5: HPV Is Treatable
Fact:
HPV alone is not treatable. However, the HPV condition, precancerous lesions, and genital warts can be treated with topical medications and other therapies. It is also important to be vaccinated and to undergo regular screening.
Explanation:
In most cases, the immune system eventually clears the virus within 2 years. When infections are persistent, medical interventions involve manipulating symptoms and complications. Most dangerous HPV strains are preventable, and vaccination can significantly reduce your risk.
Myth 6: HPV Is Only Spread to Promiscuous People
Fact:
HPV is not the result of having lots of sexual partners – anyone who is sexually active can contract the virus. It’s not lifestyle, it’s exposure.
Explanation:
Because the virus is so widespread, even those in long-term, monogamous relationships can have HPV. That is because the virus can lay dormant for years. Managing your risk requires regular health check-ups and open communication with your healthcare providers.
Myth 7: Genital Warts Lead to Cervical Cancer
Fact:
Genital warts are usually caused by low-risk strains of HPV and thus are not cancer-associated. Strains at high risk for producing cervical cancer warts are rare and often asymptomatic.
Explanation:
Although genital warts can be distressing, they’re not a direct indicator of cancer. However, regular screenings are crucial for everyone, regardless of whether they have genital war
Myth 8: HPV Screening is Not Necessary for Lesbians
Fact:
Lesbian and bisexual women are also at increased risk for developing HPV through skin-to-skin contact during sexual activity.
Explanation:
A review of the literature suggests that lesbians have a much higher HPV prevalence compared with heterosexual women. So, it’s important for all sexually active people to get regular cervical cancer screening, regardless of sexual orientation.
Myth 9: Cancer Means an Abnormal Pap Test
Fact:
Having an abnormal Pap test doesn’t directly mean you have cancer. This indicates that there are cellular changes in your cervix. Injury, inflammation, low-risk HPV, or infections can cause these changes.
Explanation:
Abnormal results must be followed up with other testing, such as colposcopy or biopsy, to determine the cause. Early detection leads to the treatment of precancerous changes and prevents cancer.
.png)
Take Action This January: Cervical Health Awareness Month
January is Cervical Health Awareness Month, a time to highlight the importance of preventive care. This month reminds us to schedule screenings, talk with the cancer care specialist about vaccination, and educate others about HPV’s risks and prevention.
Take Action:
-
Schedule your Pap smear and HPV test when it’s due.
-
If you are an adolescent or young adult, talk to your doctor about the HPV vaccine.
-
Help dispel myths and open conversations about HPV by sharing accurate information with friends and family.
Your best defense against HPV is taking proactive steps to learn what you can do to protect yourself and others from HPV. This includes educating yourself, addressing common myths, and providing clear, factual information. Regardless, knowledge is crucial for protecting your health.
FAQ's
Of course, high-risk HPV strains can cause cancer in the anal, throat, and penile areas. Vaccination awareness is important to prevent HPV-related cancers for everyone.
Although HPV doesn’t usually affect pregnancy, it can lead to genital warts or, rarely, affect the baby at birth—monitoring and guidance from your doctor will be needed in such cases.
Up to 80% of HPV infections, in most cases, will clear themselves within 2 years. However, high-risk strains can survive, and you will require regular medical follow-ups to control risks.





















 7 Min Read
7 Min Read







.png)