
Pelvic floor disorders after childbirth are a significant concern for many new mothers. These disorders can lead to discomfort, pain, and emotional distress, affecting a woman's quality of life. Understanding the treatment and prevention of pelvic floor disorders after childbirth is crucial for new mothers. This blog will explore various aspects of pelvic floor disorders, including their causes, treatments, and preventive measures. We will also discuss how Manipal Hospitals Patiala can support women experiencing pelvic floor issues.
Synopsis
- Common Symptoms of Post-Childbirth Pelvic Floor Problems
- Treatments for Pelvic Floor Problems After Childbirth
- Preventing Pelvic Floor Issues
- Psychological Impact of Pelvic Floor Disorders
- Role of Hormones in Postpartum Pelvic Health
- Lifestyle Adjustments for Recovery
- Specific Pelvic Floor Therapies
- Long-term Implications and Maintenance
- Nutrition and Hydration for Pelvic Health
- Role of Partner Support
- Differences Between Vaginal and C-section Recovery
- Exercise and Fitness Guidance Postpartum
- Pelvic Floor Disorders in the Context of Multiple Pregnancies
- Postpartum Pelvic Floor Check-Up Recommendations
- Conclusion
Common Symptoms of Post-Childbirth Pelvic Floor Problems
Every woman’s experience is different, but some common symptoms of pelvic floor problems after childbirth include:
-
Incontinence: Trouble controlling urine or stool, which might include leakage, urgency, or difficulty fully emptying the bladder.
-
Pelvic Pain and Pressure: This might include pain during sex, lower back pain, and a feeling of heaviness or pressure around the pelvic area.
-
Pelvic Organ Prolapse (POP): When weakened muscles allow organs like the bladder or rectum to press into the vagina, which can cause discomfort or a dull ache.
-
Other Symptoms: Constipation, difficulty passing stool, pain around the vaginal opening, and a gap between the abdominal muscles (called diastasis recti).
Treatments for Pelvic Floor Problems After Childbirth
Pelvic floor therapy is a common treatment option, often guided by a physical therapist. Therapy may include:
-
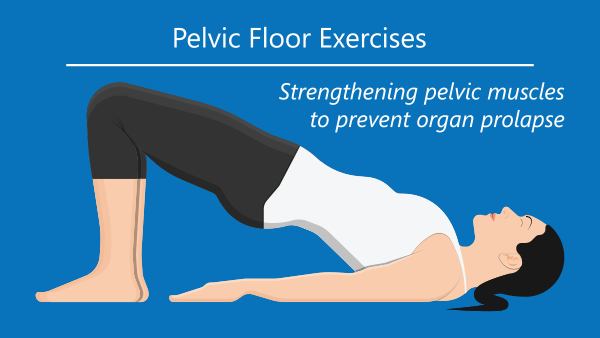
Pelvic Floor Exercises: Kegels and other exercises can strengthen or relax the muscles as needed.
-
Posture and Body Awareness: Learning new ways to move and sit can help relieve symptoms.
-
Behavioral Adjustments: Tips on managing or preventing urine or stool leakage.
-
Breathing Techniques: Certain breathing practices can help ease symptoms.
-
Biofeedback: Uses feedback devices to encourage correct muscle responses.
Many postpartum pelvic floor issues improve over weeks or months, but if symptoms are affecting your daily life, don’t wait to talk to our best gynaecologists in patiala.
Preventing Pelvic Floor Issues
Taking care of your pelvic floor before childbirth can help reduce problems later. Some helpful steps include:
-
Doing Kegels: Regular Kegel exercises can strengthen the pelvic floor muscles.
-
Eating a high-fiber diet: This can prevent constipation and avoid straining muscles.
-
Avoiding Heavy Lifting: Reduces unnecessary pressure on the pelvic muscles.
-
Not Smoking: Smoking can weaken pelvic muscles and increase coughing, which strains the area.
Psychological Impact of Pelvic Floor Disorders
Many women experience emotional and psychological distress due to incontinence, pain, or prolapse. The psychological effects of pelvic floor disorders can include anxiety, depression, and body image issues. Coping mechanisms such as joining support groups, seeking therapy or counselling, and engaging in open conversations with loved ones can help manage these feelings. It's important to address the psychological impact to provide a holistic approach to treatment.
Role of Hormones in Postpartum Pelvic Health
Hormonal changes significantly affect muscle recovery, tissue elasticity, and dryness. Estrogen levels, in particular, play a crucial role in pelvic floor recovery. Hormonal therapies can aid in healing, and breastfeeding can sometimes delay recovery due to hormonal influences. Understanding the role of hormones can help in managing pelvic floor disorders effectively.
Lifestyle Adjustments for Recovery
Making lifestyle adjustments can significantly aid in the recovery from pelvic floor disorders after childbirth. Ergonomic practices, such as maintaining proper posture during breastfeeding, can prevent further strain on the pelvic floor. Safe physical activities and managing lifting and childcare tasks without straining the pelvic floor are essential for recovery.
Specific Pelvic Floor Therapies
-
Electrical stimulation therapy.
-
Vaginal pessaries: for prolapse management.
-
Manual therapy techniques: provide relief and aid recovery.
Long-term Implications and Maintenance
Ongoing pelvic floor care is crucial even after recovery. Untreated pelvic floor disorders can lead to worsening prolapse or chronic pain. Maintaining pelvic health during menopause and understanding the long-term implications of pelvic floor disorders can help in planning for future health.
Nutrition and Hydration for Pelvic Health
Diet plays a critical role in recovery and symptom management. Foods that promote muscle repair and tissue healing, staying hydrated to avoid constipation, and supplements like collagen or magnesium can support recovery. Proper nutrition and hydration are essential for maintaining pelvic health.
Role of Partner Support
Partner support is vital in managing pelvic floor disorders after childbirth. Partners can assist in daily tasks, improve intimacy post-childbirth, and attend doctor or therapy visits together. Open conversations and shared responsibility can significantly improve recovery and relationships.
Differences Between Vaginal and C-section Recovery
|
Aspect of Recovery |
Vaginal Delivery |
C-section Delivery |
|
Recovery Time |
Typically 4-6 weeks |
Typically 6-8 weeks |
|
Pain and Discomfort |
Perineal pain, soreness, and swelling |
Incision pain, soreness, and potential infection |
|
Mobility |
Generally quicker return to normal activities |
Slower return to normal activities due to incision |
|
Hospital Stay |
1-2 days |
3-4 days |
|
Bleeding |
Postpartum bleeding (lochia) for up to 6 weeks |
Postpartum bleeding (lochia) for up to 6 weeks |
|
Pelvic Floor Impact |
Higher risk of pelvic floor disorders |
Lower immediate risk, but still possible |
|
Scar |
No external scar |
Visible scar on the abdomen |
|
Infection Risk |
Lower risk of infection |
Higher risk of infection at the incision site |
|
Physical Activity |
Can resume light activities sooner |
Need to avoid heavy lifting and strenuous activities longer |
|
Emotional Impact |
May experience emotional highs and lows |
May experience emotional highs and lows, plus feelings about the surgery |
|
Breastfeeding |
Generally easier to start immediately |
May be delayed due to recovery from surgery |
Exercise and Fitness Guidance Postpartum
Safe postpartum exercises beyond Kegels, such as yoga or Pilates, can aid in recovery. It's important to recognize warning signs to stop exercising, like increased prolapse symptoms, and follow a timeline for resuming higher-intensity workouts. Proper exercise guidance can help women transition back to regular physical activity safely.
Pelvic Floor Disorders in the Context of Multiple Pregnancies
Multiple pregnancies can have a cumulative effect on pelvic floor health. Understanding how subsequent pregnancies affect pelvic floor health and taking preventive care between pregnancies can help in managing pelvic floor disorders effectively.
Postpartum Pelvic Floor Check-Up Recommendations
Regular postpartum pelvic exams are crucial for early detection and management of pelvic floor disorders. Understanding the timeline for these evaluations, what to expect during them, and the importance of follow-ups even if symptoms are mild can aid in maintaining pelvic health.
Conclusion
Pelvic floor issues are common after childbirth but aren’t something you just have to "live with." These issues—like incontinence, pain, and pelvic organ prolapse—are treatable. By recognizing the symptoms and seeking help, you can improve your comfort, function, and quality of life. Preventive care and early treatment can also help you recover more effectively and avoid long-term problems. Always feel empowered to discuss any postpartum symptoms with your doctor; they are there to help you.
Manipal Hospitals Patiala offers comprehensive support for women experiencing pelvic floor issues. Their team of specialists provides personalized care, including advanced diagnostic and treatment options. Women can benefit from their expertise in managing pelvic floor disorders, ensuring a holistic approach to recovery and well-being.
FAQ's
Light pelvic floor exercises, like Kegels, can often begin a few days after delivery, but consult your doctor first.
Yes, even with a C-section, pregnancy can weaken the pelvic floor muscles.
Improvement can be seen in a few weeks to a few months with consistent pelvic floor therapy.
Mild symptoms may improve, but persistent issues typically require treatment.
Pelvic floor therapy, relaxation techniques, and using lubrication can help ease pain during sex.
Regular pelvic floor exercises, avoiding heavy lifting, and maintaining a healthy diet can help prevent issues.
If your symptoms are severe or affect your daily life, it's important to see a doctor.
Medications may help manage certain symptoms, but pelvic floor therapy is typically more effective.
Yes, regular pelvic floor exercises like Kegels can help maintain muscle strength and prevent future issues.



















 4 Min Read
4 Min Read











