-
Book Appointments &Health Checkup Packages
- Access Lab Reports
-
-
Book Appointments &Health Checkup Packages
-

Emergency Contact Number
-
Centre of Excellence
Centre of Excellence
- Robotic Spine - MIRSS
- Bariatric Surgery - MIBS
- Head and Neck - MIHNS
- Children's Airway & Swallowing Centre - CASC
- Accident and Emergency Care
- Cancer Care/Oncology
- Cardiology
- Cardiothoracic Vascular Surgery
- Dialysis
- Gastrointestinal Science
- Interventional Neuroradiology
- Laparoscopic Surgery
- Liver Transplantation Surgery
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Organ Transplant
- Orthopaedic Robotic Surgery
- Orthopaedics
- Paediatric And Child Care
- Proctology
- Rheumatology
- Shoulder, Arthroscopy And Sports Injury
- Spine Care
- Urology
- Woman and Child Care Centre
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Bariatric Surgery | Weight loss surgery
- Bone Marrow Transplantation
- Children’s Airway & Swallowing Centre
- Clinical Haematology
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Genetics
- Geriatric Medicine
- GI Surgery
- Growth and Hormone
- Gynaec Oncology
- Hand and Upper Limb Surgery
- Hand Surgery
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- IVF and Infertility
- Kidney Transplant
- Laboratory Medicine
- Lactation
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Neuro-Otology (Vertigo & Hearing Clinic)
- Nocturnal Dialysis
- Nuclear Medicine
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Cancer Care
- Paediatric Cardiology
- Paediatric Endocrinology
- Paediatric General Surgery
- Paediatric Infectious Disease
- Paediatric Intensive Care Unit
- Paediatric Neurology
- Paediatric Surgery
- Paediatric Urology
- Pain Management
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pediatric Bone Marrow Transplant
- Pharmacy
- Physical Medicine and Rehabilitation
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Preventive Health Check-Up
- Psychiatry
- Psychology
- Pulmonary Medicine
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Radiotherapy (Oncology Radiation)
- Rehabilitation Medicine
- Renal Sciences
- Reproductive Medicine
- Robotic Assisted Surgery
- Senior Care Program
- Speech Therapy
- Sports Medicine
- Surgical Gastro
- Surgical Oncology
- Thoracic Surgery
- Transfusion Medicine
- Trauma Care
- Vascular and Endovascular Surgery
Speciality Clinics
- Angioedema Clinic
- Attention Deficit Hyperactivity Disorder (ADHD) Clinic
- Autism Clinic
- Breast Cancer Clinic
- Cystic Fibrosis Clinic
- Diabetic Care Clinic
- Epilepsy Clinic
- Fibroid Clinic
- Gait & Posture Clinic
- Hair Transplantation Clinic
- Head and Neck Clinic
- Healthy Weight Clinic
- Heart Care Clinic
- Heart Failure Clinic
- Lifestyle Clinic
- Liver Clinic
- Lymphedema Clinic
- Neuromuscular Clinic
- Shoulder Clinic
- Stroke Care Clinic
- Urgent Neuro Care Clinic
- Varicose Veins Clinic
- Vitiligo Clinic
- Voice Clinic
- Doctors
- Hospitals
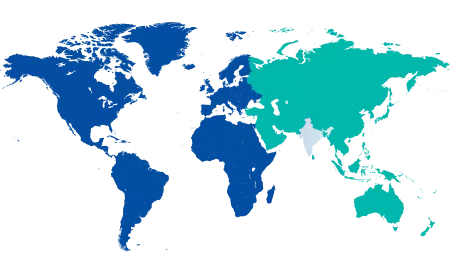
- International Patients
-
-
-
Search
-
- Self Registration
- In-Patient Deposit
- Mars - Ambulance
- Home Care
- Privilege Card
- Organ Donation
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Teleradiology
- Manipal Insider
- Referral Program
- Careers
- Contact Us
Corporate & Investor Relations
Appointment Helpline